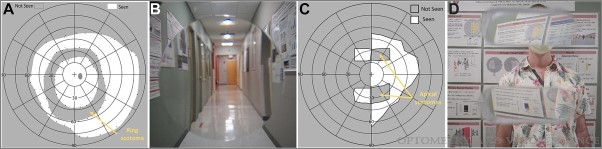
The effects of blind spots caused by eye disease, injury, or surgery can be difficult to understand and even more difficult to illustrate. New research from Eli Peli, MSc, OD, offers a glimpse of the world as seen by people with blind spots.

People frequently develop blind spots, or scotomas, in their vision as a result of retinal diseases such as macular degeneration, early glaucoma, and others. According to vision rehabilitation researcher Eli Peli, MSc, OD, the Moakley Scholar in Aging Eye Research at Mass Eye and Ear, the experiences of these individuals is not adequately captured by prevailing models in current medical literature and websites. In a recently published paper in Optometry and Vision Science, Peli and colleagues use videos and photos of highways, hallways and everyday indoors environments to offer a glimpse of the world seen by people with blind spots due to eye disease. In this Q&A, he describes the challenge of simulating blind spots and how his new model might impact future study and clinical care for patients rehabilitating their vision.
What exactly are blind spots, and how might they impact a person’s daily life?
If part of our wide visual field becomes blind due to disease, injury or surgery, then you have a blind spot. Every healthy person already has one blind spot in each eye, which is invisible because it is compensated for by vision by the other eye. If you simply cover one eye, you will not note this blind spot. But if you move your finger slowly and search for it, you can detect when the finger disappears into the blind spot. The finger simply disappears. When people talk about blind spots, they frequently think that it looks like a black spot over the field of view. We know that this model is flawed, but you will find these diagrams in most textbooks and websites. The point of this project is to highlight that blind spots are not black spots or grey spots or any other visible spot over the scene. They are areas where no seeing takes place, much like being unable to see behind your head. We think about how you would describe or illustrate what you see behind your head.
Why are simulations of eye disease so useful to researchers, clinicians, and patients?
If researchers or clinicians do not understand what a patient sees, it’s unlikely they will create a device or method that will help patients. When patients see inaccurate simulations on websites and articles, they might think, “Well this is not how I see.” They are bewildered and may think that the disease described does not apply to them. This can interfere with them seeking and accepting the necessary care.
How does your work disprove the prevailing static black spot model of blind spots? How did you create more realistic simulations of an invisible blind spot?
Most existing blind spot simulations are static; they are just a picture. But our vision is not static. Even if you are looking straight ahead at the world, moving cars and people will disappear into your blind spot and later reemerge from it.
A few simulations include videos, but they just put a black spot in the middle of a video. Most simulations provide illusions like this, but these are not accurate. They do not cover the more common type of movement which is the movement of the eye (and with it the blind spots) over the visual scene.
I included two types of movements in these new simulations: a moving objects within the static world, and the movement of the eye’s invisible blind spot within this world due to eye movements. Even if the blind spot is not visible, the distortions it causes when you move your eyes can be made noticeable. We all normally have rapid eye movements, or saccades, about 3 per second, yet we do not see the effects of these movements with or without blind spots. Our simulations capture how these distortions and their movements are also not noticed by the patients.
How did the previous model of blind spots using patches to cover part of a scene limit patient care for eye degeneration? How will your findings advance care in the future?
I can provide two examples: patients with macular degeneration who report blurry vision as opposed to black spots, and patients with glaucoma, who despite having measurable peripheral field losses report neither black spots nor blurriness. The glaucoma takes away a patient’s vision without them realizing, which is why it is known as the “silent thief of sight.” Patients with glaucoma are notoriously noncompliant with the eye drop medication they are supposed to use for a lifetime; only approximately 30 percent continue to use the eye drops for three months.In such cases, if we have an accurate simulation that captures a patient’s experience and use it to explain and illustrate the situation to them, they may realize why they are not seeing and their measurable vision loss. They then may become more compliant with the treatment.
You call for future research to verify this paper’s computer simulations with patients and develop improved ways to measure these blind spots. What comes next for you?
I’m currently working with an international group using replicates of visual studies to document distortions around blind spots associated with brain lesions. A lot of studies in the field have not built replication into their design, so we are happy to serve as a duplicating center for this study. We are not specifically testing the simulation described in the paper but are testing if and how patients experience visual distortions. Once we have this information, we can see if the reported distortions are similar to those created by my simulation. If so, we can start using my simulation program to better understand individual patients’ vision loss and refine the current simulations.
Throughout your career you have developed and studied innovative vision rehabilitation aids. What are some of the advances to address degenerative eye disorders that you think we should prepare for in the coming years?
The field should be going towards improving understanding of eye disease and their impact. Sometimes there is great interest in jumping to the treatment, solutions and new technologies, but rehabilitation for patients with eye disease, trauma and surgeries requires better understanding of the patient experience. I’ve come up with lots of engineering solutions, but they must be fine-tuned and evaluated using patient feedback. Restoring vision is an idealistic goal. Instead, I prefer slowly improving our understanding of the world seen by patients with eye disease to make their lives better.




I am experiencing exactly that situation in my right eye. I’ve been taking drops for about three weeks but haven’t seen much improvement.
I have multiple “blind spots” post retinal detachment repair. This causes a significant deficit in vision in that eye. Are there any aids you have developed that can help me? I am a patient in the retina service at MEEI.
Thankyou for this information. We appreciate receiving it.