Mass Eye and Ear is celebrating its 200th anniversary, and the Focus blog each month will have stories on the hospital’s past, present and future. In February, Focus is spotlighting some of the ophthalmology department’s most significant achievements in clinical care, research and education. Learn more in an in-depth Advances in Motion article.

More than 80 Years of Excellence in Glaucoma Care, Teaching and Research
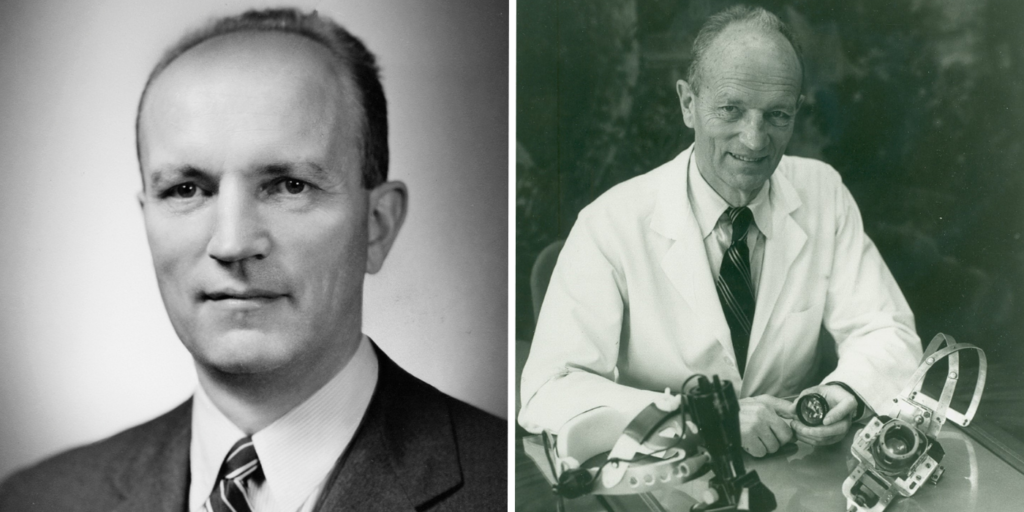
In 1940, Paul A. Chandler, MD, who would go on to become a national leader in the diagnosis and management of glaucoma, joined the staff at Mass Eye and Ear, where he developed a busy glaucoma practice.. In 1943, W. Morton Grant, MD, joined the Howe Laboratory at Mass Eye and Ear, and quickly became Dr. Chandler’s most frequent research collaborator. Together, the two friends and colleagues helped transform both the clinical and investigative fields of glaucoma.

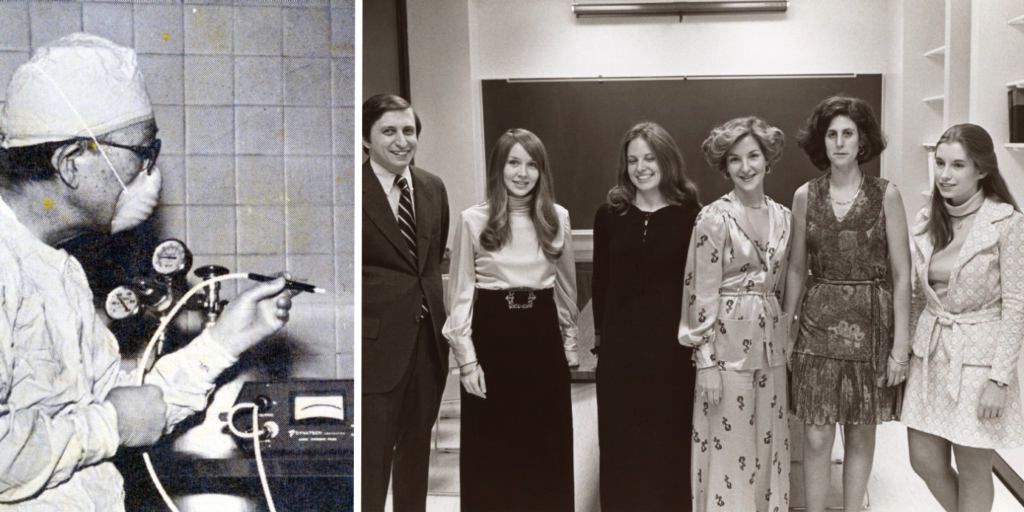
Drs. Chandler and Grant were also highly respected educators and mentors, dedicated to teaching the next generation of glaucoma specialists. When they met weekly for lunch to discuss interesting cases and challenges, they encouraged trainees to bring their own bagged lunch and join them for the discussions. In 1982, fellows who trained under the pair founded The Chandler-Grant Society to carry on their legacy. One such trainee was the late David Epstein, MD, who would go on to become one of the most influential leaders in glaucoma care and research in the modern era. Dr. Epstein, who went on to lead the Mass Eye and Ear Glaucoma Service after Dr. Grant, believed learning directly from the patient’s presentation, investigating first in the clinic, and if that didn’t solve the issue, taking the question to the laboratory to determine the cause and treatment.

Decades later in 2021, working with international collaborators from more than 10 different countries, medical geneticist and glaucoma specialist Janey Wiggs, MD, PhD, identified over 120 novel genetic risk factors for various forms of glaucoma. This study, the largest of its kind, may help lead to the discovery of new glaucoma treatments.
Charles L. Schepens, MD: Retina Pioneer and Innovator
In 1947, Charles L. Schepens, MD, joined Mass Eye and Ear, and soon after established the world’s first retina service and retinal disease fellowship program. Since then, the Retina Service has grown to be one of the largest in the country, providing the most advanced medical and surgical care and access to cutting-edge clinical trials. Mass Eye and Ear retinal researchers and clinician-scientists have been at the forefront of the most transformative advances in retinal care, including photodynamic therapy, the first FDA-approved treatment for wet age-related macular degeneration (AMD), and anti-vascular endothelial growth factor (VEGF) therapy for AMD, diabetic retinopathy and other retinal disorders.
Dr. Schepens is widely known as the father of modern retinal surgery. He pioneered many surgical procedures and also developed numerous ophthalmic instruments, including several different ophthalmoscopes, a tool that allows you to view the back of the eye to look at the health of the retina. His devices and surgical techniques have been credited with raising the success rate of retinal reattachment surgery from 40% to 90%.
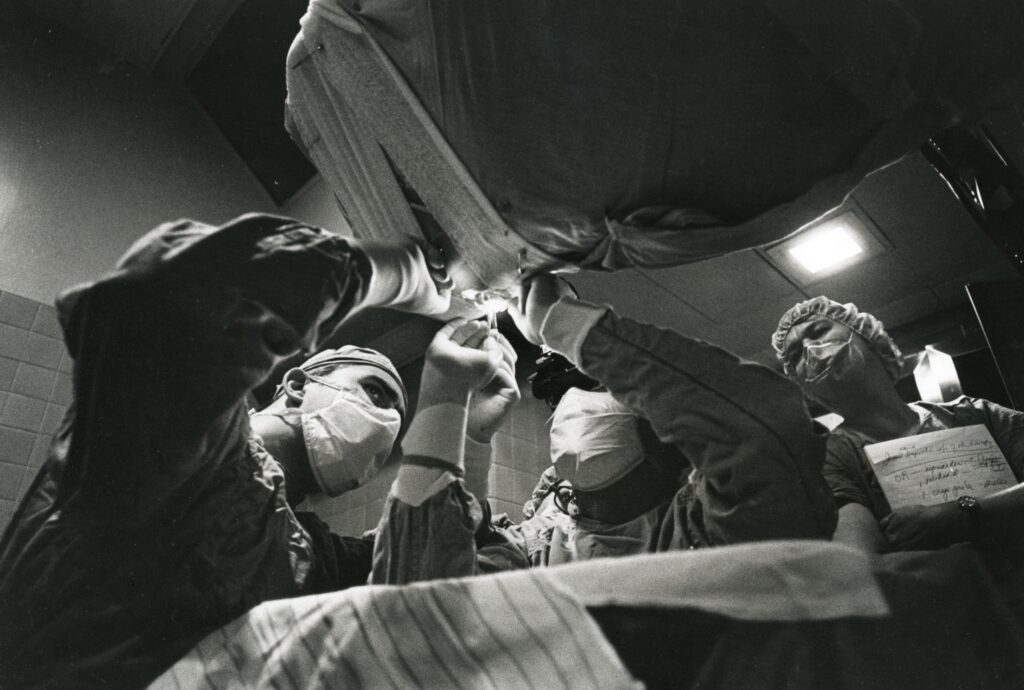
Mass Eye and Ear retinal surgeon Hal Mackenzie Freeman, MD, continued Dr. Schepens legacy of pioneering retinal surgery procedures. In 1965, Dr. Freeman published a paper with Dr. Schepens on an inverted (upside-down) operating table they designed to fix giant retinal tears. This table suspended patients face down above the surgeon and allowed for gravity to unfold the giant retinal tear, thus making it operable for the surgeon. The prototype of the giant retinal tear operating table is now at the Smithsonian Institute in Washington.
Claes H. Dohlman, MD, PhD: Cornea Research Pioneer and Visionary
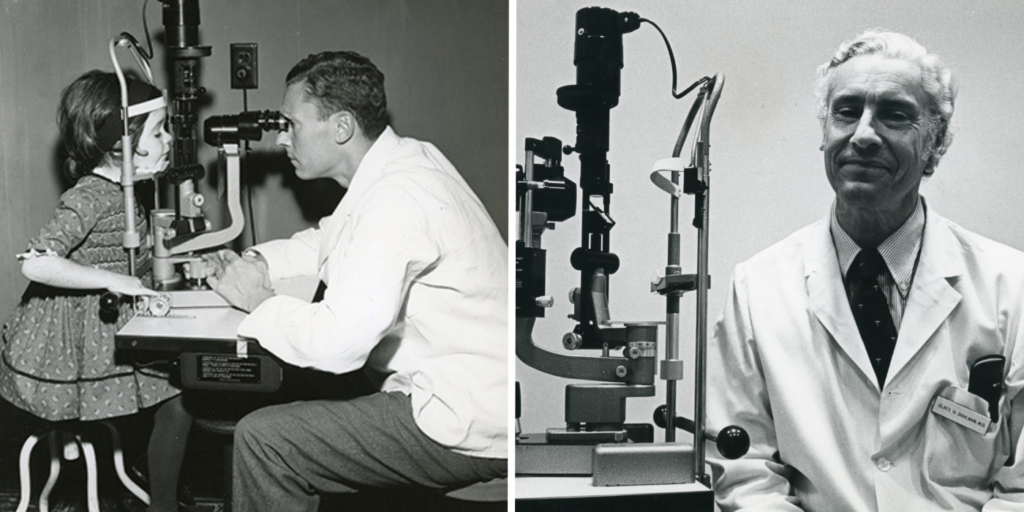
In a career that now spans seven decades, Claes Dohlman, MD, PhD, is widely considered the father of modern corneal science. In 1958, Dr. Dohlman joined Mass Eye and Ear, where he founded the Cornea Service—the first cornea subspecialty clinic in the world—and the first-ever cornea fellowship. Under Dr. Dohlman’s leadership, the Cornea Service has grown to be one of the largest and most renowned in the world. Cornea research started at Mass Eye and Ear has led to new treatments for a range of diseases, including stem cell transplantation for ocular surface reconstruction and the Boston Keratoprosthesis (K-Pro, an artificial cornea).
First developed by Dr. Dohlman in 1965, the Boston KPro was approved by the FDA in 1992 and is still the most widely used and successful artificial cornea to date. Today, clinician-scientists at Mass Eye and Ear, led by Eleftherios Paschalis, PhD, and Dr. Dohlman’s grandson, Thomas Dohlman, MD, work to further advance this technology, including the development of the ‘Lucia’ KPro which offers improved cosmetic appearance for patients.
50 Years of Proton Beam Irradiation
Developed in 1975 by Evangelos Gragoudas, MD, proton beam irradiation (PBI) is a focused form of
radiation that is particularly effective for treating tumors near critical parts of the eye. The therapy delivers a precise beam of radiation to the tumor, thereby limiting damage to the surrounding healthy tissues.
Under the mentorship of Dr. Schepens, Dr. Gragoudas began work on PBIas an alternative to enucleation for choroidal melanoma. Nearly 50 years of follow-up studies show that PBI has the lowest local recurrence rate of any radiation therapy and is currently one of the most effective therapies for treating intraocular tumors.
25 Years of Photodynamic Therapy
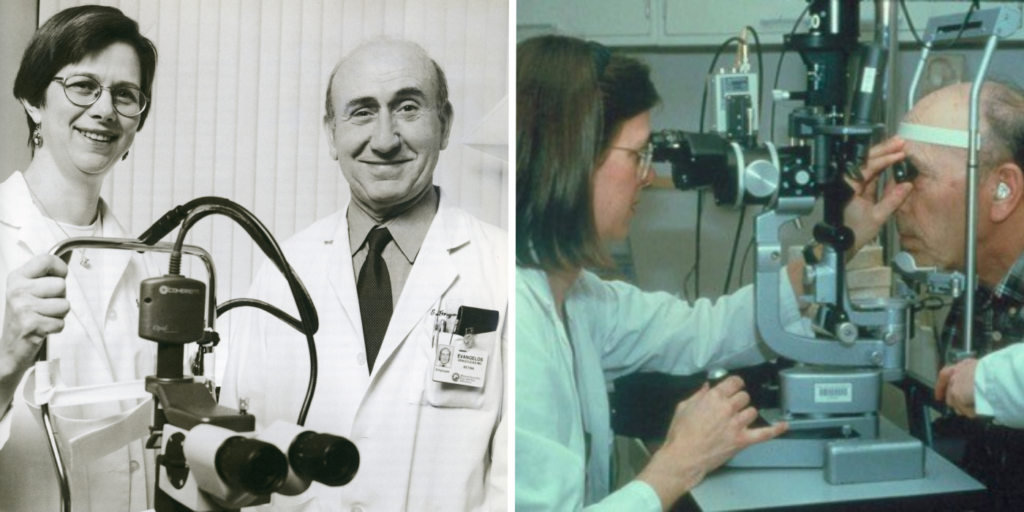
Dr. Gragoudas and Joan W. Miller, MD, both internationally recognized experts on retinal disorders, pioneered studies for the use of photodynamic therapy, a treatment that involves light-sensitive medicine and a light source to destroy abnormal cells. Based on these Mass Eye and Ear studies, photodynamic therapy using verteporfin (Visudyne®) became the first approved therapy to treat neovascular retinal disease (abnormal blood vessel growth in the retina) and slow vision loss in patients with AMD.
25 years of Anti-VEGF Treatment for Retinal Disorders
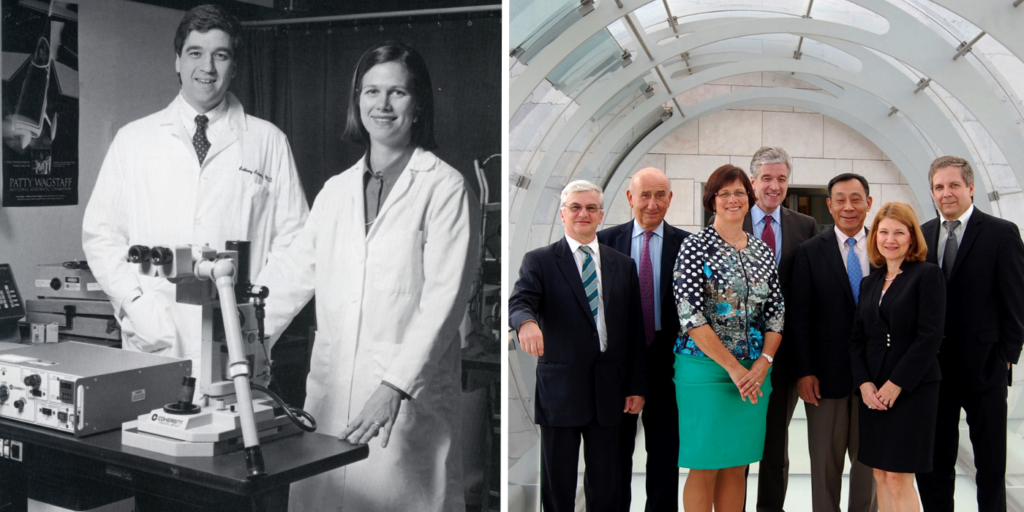
In the 1990s, Mass Eye and Ear researchers Drs. Miller, Gragoudas, Anthony Adamis, MD and Patricia A. D’Amore, PhD, MBA, worked in collaboration with researchers at Joslin Diabetes Center and Genentech (a biotechnology company) to identify VEGF as the main cause ofthe formation of new blood vessels in the eye (angiogenesis). This formation is the root of several blinding retinal disorders, including AMD and diabetic retinopathy. The researchers demonstrated that blocking VEGF could suppress the growth of the blood vessels., leading to a new group of anti-VEGF drugs, which first became available in the United States in 2003 with the introduction of pegaptanib (Macugen®) for neovascular AMD. There are now numerous approved anti-VEGF drugs, and millions of people receive anti-VEGF injections annually around the world.
In recognition of their transformational clinical research, the team was awarded the 2014 António Champalimaud Vision Award, the highest distinction in ophthalmology and visual science.
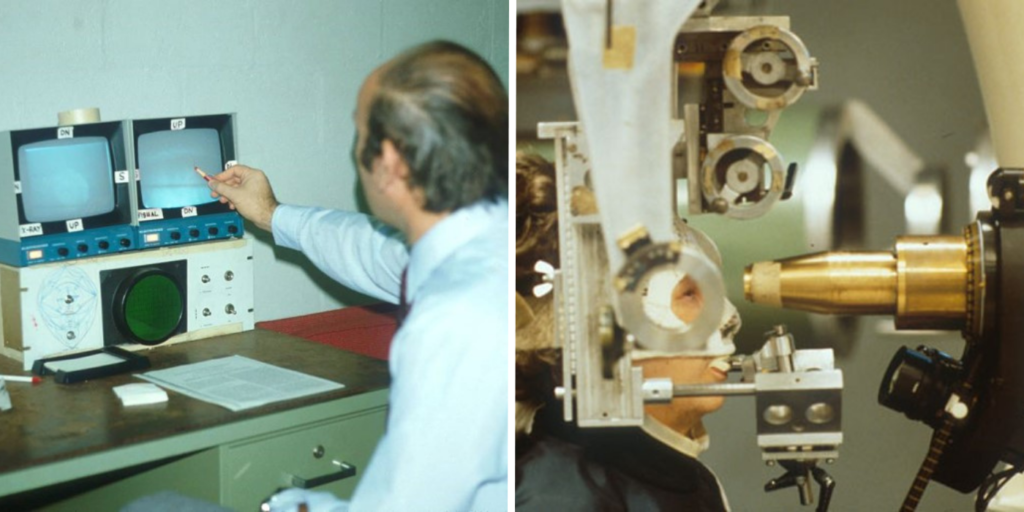
25 years of Optical Coherence Tomography

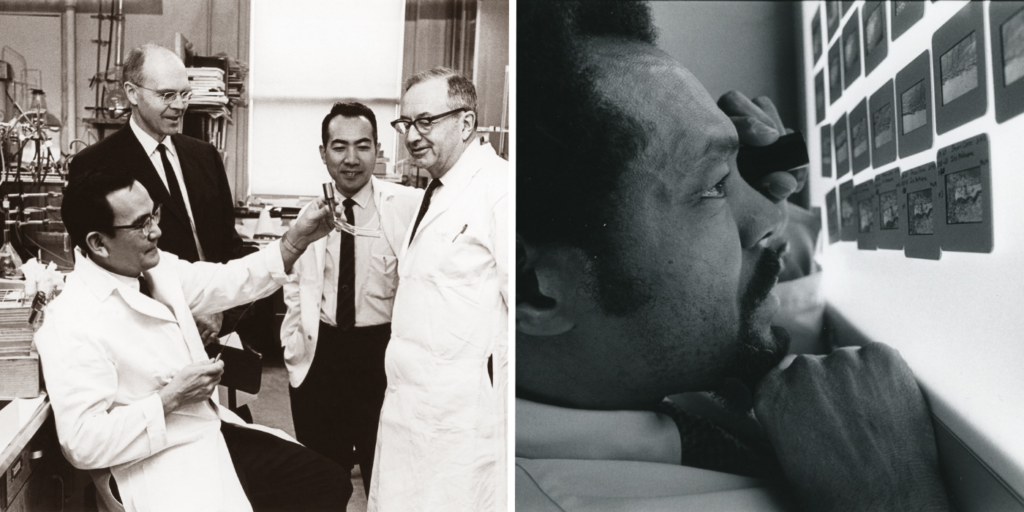
Researchers at Mass Eye and Ear, Mass General Hospital, and MIT co-discovered optical coherence tomography (OCT), the most widely used non-invasive imaging tool in retina care. David Huang, MD, PhD, was a graduate student at Harvard Medical School/MIT Health Sciences and Technology program, working at Mass Eye and Ear when he published his first paper on OCT with co-inventors James Fujimoto, SM, PhD, and Eric Swanson, SM, and former Mass Eye and Ear researcher Joel Schuman, MD.
The development of OCT imaging completely revolutionized ophthalmic care by allowing clinicians to rapidly detect and then treat retinal diseases. As OCT imaging technology has advanced, it has become increasingly used for a range of eye disorders including AMD, diabetic retinopathy, retinal vein occlusions and uveitis, among others.
Excellence in Education
Mass Eye and Ear is the primary teaching hospital of Harvard Ophthalmology, led by its chair, Dr. Joan Miller. Medical students, residents and fellows receive world-class training in comprehensive ophthalmology and all the ophthalmic subspecialties, and students and post-doctoral fellows receive training in internationally renowned laboratories. Harvard Ophthalmology prides itself on training the next generation of ophthalmology and vision research leaders, and about one in five current ophthalmology department chairs in the U.S. and Canada are alumni.
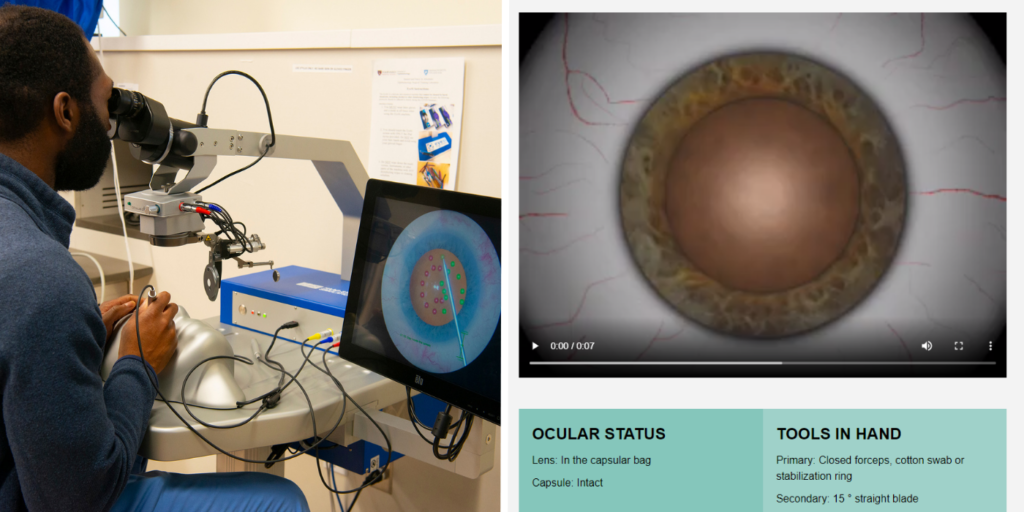
The department also leads the nation in developing an innovative and challenging cataract training program for ophthalmology residents. The first national cataract surgery course launched in 2005 and is held annually since. In 2012, former faculty members John I. Loewenstein, MD, and Bonnie An Henderson, MD, created the Cataract Master, a digital cataract surgical training tool that is now available nationally to American Academy of Ophthalmology members.
In 2017, Mass Eye and Ear established the Samuel and Nancy Jo Altschuler Ophthalmology Surgical Training Laboratory thanks to the generous give of the Altschuler family honoring Lucy Young, MD, PhD. The facility features state-of-the-art surgical training equipment that allows Harvard Ophthalmology residents, Mass Eye and Ear Fellows, and practicing surgeons to refine their surgical skills in a realistic preoperative environment.
Lucien Howe Library of Ophthalmology and Frederick A. Jakobiec, MD, DSc, Education and Information Center
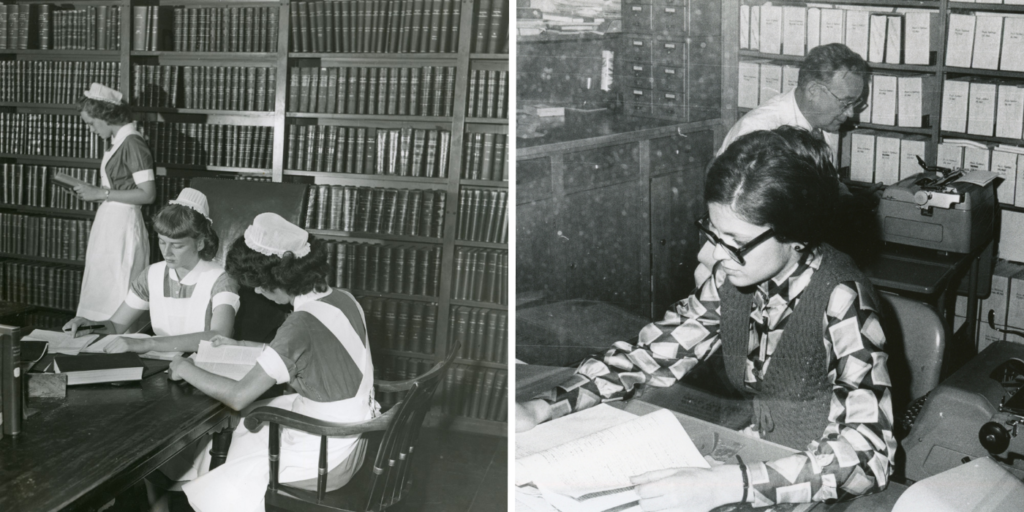
For nearly 150 years, the Libraries of Mass Eye and Ear have provided the highest quality of information resources and services available for evidence-based decision making for patient care and research. The original Mass Eye and Ear library was established in 1876, and in 1926, when the Lucien Howe Library of Ophthalmology at Mass Eye and Ear was founded, the two libraries merged.
In 1986, the library moved into its new space on the third floor of 243 Charles Street, where it remains today. At that time, the library was equipped with public-access computers and the hospital’s first fax machine. To reflect the funding that built the new library, the name was changed to The Libraries of the Massachusetts Eye and Ear Infirmary: The Lucien Howe Library of Ophthalmology, The Leroy A. Schall Library of Otolaryngology, and the Abraham Pollen Archives and Rare Book Library.
In 2019, the late Frederick A. Jakobiec, MD, DSc, made a bequest of $1 million to support renovations and improvements to the library, now known as the Frederick A. Jakobiec, MD, DSc, Education and Information Center. A lifelong learner and devoted educator, Dr. Jakobiec was former Chair of Harvard Ophthalmology and former Chief of Ophthalmology at Mass Eye and Ear.
Ophthalmology Research Laboratories
Mass Eye and Ear unites researchers from three historical laboratories: the Howe Laboratory, Schepens Eye Research Institute, and the Berman-Gund Laboratory for the Study of Retinal Degenerations.
Howe Laboratory
In 1926, Frederick H. Verhoeff, MD, Mass Eye and Ear’s first full-time researcher and pathologist, established the first endowed ophthalmic research unit, the Howe Laboratory, at Mass Eye and Ear. David G. Cogan, MD, directed the laboratory from 1940 to 1974, and it became a hub for translational research.
Berman-Gund Laboratory for the Study of Retinal Degenerations
Founded in 1974 under the leadership of the late Eliot L. Berson, MD, and established by philanthropists Gordon Gund and Bernard Berman and supported by the Foundation Fighting Blindness, the Berman-Gund Laboratory for the Study of Retinal Degenerations conducts multidisciplinary research on these disorders. To date, its researchers have helped discover more than 20 of the genes which harbor mutations that cause these disorders and are currently exploring new methods of treatment including gene augmentation therapy.
Schepens Eye Research Institute of Mass Eye and Ear
Originally called the Retina Foundation, Schepens Eye Research Institute of Mass Eye and Ear was founded in 1950 by pioneering retinal surgeon Dr. Charles Schepens. In 2011, Mass Eye and Ear joined forces with Schepens Eye Research Institute to create the world’s largest ophthalmology research institution. This collaboration is working to translate laboratory research into better treatments and new cures for blinding diseases.
Today, Schepens Eye Research Institute and the Howe Laboratory are led by Dr. Pat D’Amore, who plays a vital role in shaping research goals, overseeing faculty development, and building collaborative relationships. These storied laboratories are an important part of Mass Eye and Ear’s research history and future, although the current ophthalmology research efforts are organized around multidisciplinary Centers of Excellence and Institutes, rather than the historic laboratories, to allow clinicians, educators, investigators, trainees and laboratories to come together to focus on a specific ophthalmic disorder or scientific discipline.
Looking to the Future
From a humble one-room clinic in Boston 200 years ago to a leading institution of Harvard Ophthalmology that has driven some of the biggest discoveries in the field, Mass Eye and Ear is constantly evolving yet remains steadfast in its mission to eradicate blindness and provide premier patient care, while training the next generation of leaders in the field. This bicentennial celebration marks not an end, but a promise—a promise of more cures for patients, more lives touched and more hope kindled, as Mass Eye and Ear embarks on the next chapter of its enduring mission.
Mass Eye and Ear’s Department of Ophthalmology is focused on providing clinical innovations and care to areas where the greatest unmet needs still exist, including retinal degenerations, macular degenerations, diabetic eye disease and glaucoma. Other important clinical areas include the cornea and ocular surface, oncology, immunology, infectious disease and vision rehabilitation. As technology continues to advance, Mass Eye and Ear ophthalmology researchers are also pursuing a range of promising new areas, including artificial intelligence, big data, genetics and gene-based therapy, imaging and other diagnostic technologies.
This story originally appeared on the Advances in Motion website and has been edited and shortened. View the full version of this story.
Learn More about Mass Eye and Ear’s History



