Program offers parents virtual training and resources to tackle problems that might arise at home following discharge, such as with their child’s feeding tubes.
Bringing home a newborn can be a challenging time for any family. For parents whose babies had to spend months in the neonatal intensive care unit (NICU) following birth and were sent home with feeding tubes and other special needs, these challenges can be significantly magnified.
To address these challenges and give parents the tools to succeed at home, Mollie Warren, MD, of the Department of Pediatric Newborn Medicine at Brigham and Women’s Hospital recently launched a Transition to Home Program. The program was launched following years of collaboration with other colleagues within Mass General Brigham, including Christopher Hartnick, MD, director of the Division of Pediatric Otolaryngology at Mass Eye and Ear, and the Pediatric Aerodigestive Center at Mass Eye and Ear and Mass General for Children.
“A lot of people don’t realize, you think at discharge that the NICU journey is over and that’s not the case at all,” Dr. Warren, a Brigham and Women’s pediatrician and director of the Transition to Home Program told WCVB in a recent interview. “Really that’s when the hard work begins.”
Dr. Hartnick added to WCVB: “To be in the hospital for a couple of months is so very hard, which was the reason to say, ‘would the parents like to have the competencies to be considered to go home?’ I think it’s incredibly empowering for those families.”
Virtual program aimed at easing stress and fears for families
Families enrolled in the new Transition to Home Program log their newborn’s daily progress such as weight, feeding schedule and diaper changes in their MyChart app which connects to an Epic electronic health record-integrated flowsheet that is monitored by the medical team. The families participate in weekly virtual appointments with the medical team including a physician, nurse practitioner and allied health team members for feeding and growth support. Here, they discuss their baby’s progress and answer any questions. Parents also have access to a pager for more urgent questions and needs.
“Our program is entirely virtually based, and the reason why we did that is because once a baby goes home from the hospital, we want them to be able to stay home and not have to keep coming in to do a lot of doctors’ visits,” said Dr. Warren.
The program also comes with education that can help parents succeed, such as if their baby needs regular maintenance for a nasogastric feeding tube (NGT).

Prior to the program’s launch, babies might have needed to stay at the hospital for months, according to Dr. Hartnick. The new program allows them to be at home where they are more likely to do better and get into a routine.
VIDEO: Learn more about the Transition to Home Program in this segment from WCVB.
When Lila O’Connell was born at Brigham and Women’s Hospital on May 27, she seemed perfectly healthy. But one day later, she suffered a seizure and was admitted to the NICU. Tests showed she had an extremely rare neurologic disorder called ZARD, which can make swallowing difficult. As a result, Lila could not bottle- or breastfeed and needed an NGT for nourishment. Like many parents in this situation, Teresa and Norman O’Connell had no experience with inserting, replacing, cleaning or any other aspects of NGT care.
Through the Transition to Home program, Teresa and Norman got the training they needed to return home with Lila confident and comfortable. She was discharged on June 7, just 11 days after her birth.
“We didn’t want to stay any longer in the NICU,” Teresa said. “As a parent, you want your child at home with the family. Transition to Home was instrumental in making that happen. Had we not had that support, I don’t think we could have brought Lila home as soon as we did.”
Lila has also continued to receive specialized care through Mass General Brigham. She is enrolled in Brigham and Women’s Hospital’s NICU Follow-Up Program and is regularly seen at the Pediatric Aerodigestive Center
“I wouldn’t wish this on anyone, but Transition to Home and Mass General Brigham have been fantastic,” Teresa said. “I can’t say enough about her care team.”
Passport Home program born out of a parent’s frustration

Alejandra Sibemhart Roblin’s twins were born prematurely in 2021 at Brigham and Women’s Hospital, before being transferred to a NICU at a hospital closer to the family’s home. When her daughter Anna Sofia was finally discharged from the hospital after almost three months, she couldn’t drink anything and had an NGT. Alejandra recalled getting one quick training on how to use the feeding pump and tube before heading home.
“We had no idea what to do or if the tube was in the right place. We were constantly worried what would happen if she pulled the tube out, which was super easy for Anna because she was a very active girl and the first thing kids touch is their face,” Alejandra recalled. “The idea of having to come into the ER to put a new one in didn’t feel feasible at the time – it was in the height of the pandemic and there were no vaccines.”
Alejandra connected with Dr. Hartnick’s office within a few days of discharge for further follow-up. There, Alejandra met with Dr. Hartnick and Kevin Mary Callans, RN, BSN, the nurse case manager for the Pediatric Aerodigestive Center. Alejandra voiced her concerns, and Dr. Hartnick trained her on how to troubleshoot problems with the feeding tube. From there, the “Passport Home” program was informally launched.
Collaboration from around Mass General Brigham
A formal program first took root during the COVID-19 pandemic. The Brigham NICU started a “Passport Home” program for parents with infants needing NGT feeding. Parents were given an option of going home with the address of the nearest emergency department that would replace the NGT were it come out or could learn to change the NGT themselves. The NICU partnered with Dr. Hartnick’s Pediatric Aerodigestive Center, whose experts could follow-up with these children and monitor their NGTs and feeding regimens and make further safe care plans as needed.
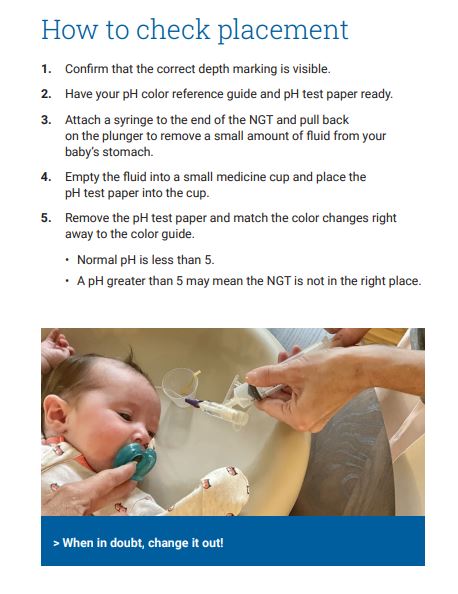
That led to development of Passport Home programs at Mass Eye and Ear, Mass General for Children and Newton-Wellesley Hospital. Dr. Hartnick and Kevin designed a teaching program that, offered parents guided training sessions along with a detailed step-by-step pamphlet and video that parents could refer to at home. Nurse educators and nurses in the Mass Eye and Ear emergency department were also trained.
Also launched out of this effort was a “Gold Pass” program, where, In the event emergency intervention is needed with a feeding tube, families enrolled in Passport Home can contact the Mass Eye and Ear 24/7 emergency department where they can be scheduled to be seen as soon as possible.
“Whether they pull up to Mass Eye and Ear at 10am or 2am, they can come in and get their tube replaced and leave,” said Kevin. “One advantage of enrolling in this program is that a parent can call ahead, rather than wait hours to be seen at their local emergency room.”
According to Kevin and Dr. Hartnick, this systemwide effort started with Alejandra and Anna. In fact, once the training program was formalized, her picture was used in the educational pamphlet given to families.
“I give Alejandra kudos, she pushed this program forward and now it is impacting children throughout the Mass General Brigham system,” said Kevin. “When the pandemic hit, it forced us as clinicians to look at these different modalities and parents like Alejandra have come up with great ideas. She deserves all the credit.”
Paying it forward

When Dr. Hartnick and Kevin thanked Alejandra for being at the forefront of this initiative, she returned the thanks right back to them.
“Thank me, I said? No, thank you, you literally gave me the tools to be free and leave the house and do things with our kids,” she recalled. “I was afraid of leaving the house and being too far from the hospital, this was an amazing gift.”
Eventually Anna outgrew the need for a feeding tube and began to take bottles. Today at almost 2 years old, Alejandra said her daughter is a funny toddler who is thriving and is “going to rule the world in whatever she wants to do.”
Now, Alejandra continues to pay it forward, and speaks with other moms when their newborns are discharged from the hospital to home with a feeding tube. She has many lessons to impart from her situation.
“I tell other parents to trust that their kids are resilient, and they are going to outgrow this. It is really hard to go through this as a family and watch your child go through it, but it makes them and the family stronger,” she said. “The last piece of advice I give is, trust the doctors. Anna would not be here if not for medicine.”



