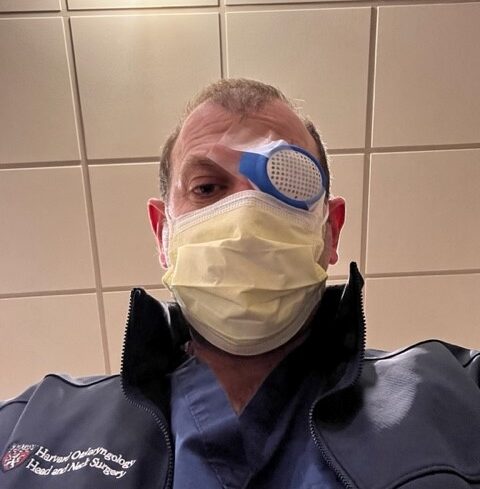
Ear, nose and throat surgeon Alex Grilli, MD, may be the first surgeon to perform and undergo a surgery at Mass Eye and Ear in the same day. His case also posed a unique challenge that would require two eye surgeons: Treating a torn retina in a patient with glaucoma.
Alex Grilli, MD, had just completed his first ENT surgery of the morning at Mass Eye and Ear when a subtle light flashed across the upper corner of his left eye. At first, the light was nothing more than a nuisance, he remembered. For all he knew, it could have been a faulty ceiling light from inside the recovery room.
As a glaucoma patient with nearsightedness, he had almost come to expect a few irregularities in his line of sight from time to time. But, as Dr. Grilli waited for the flashing to pass, the light only seemed to grow more noticeable. Then, as if out of nowhere, the peripheral vision in his eye turned completely gray.
Trying his best not to panic, Dr. Grilli texted David Solá-Del Valle, MD, his glaucoma specialist at Mass Eye and Ear. Within moments, a clinical fellow arrived to evaluate his eye. The shock in the fellow’s voice startled Dr. Grilli, and his stomach dropped as soon as he was asked when the last time he ate or drank was.
“Basically, that was surgeon talk for, ‘You need surgery, and you need it today,’” he said.
The fellow had diagnosed Dr. Grilli with a torn retina. Ivana Kim, MD, a world-renown retina specialist at Mass Eye and Ear, was paged to prepare an operation for that afternoon.
“Looking back on it now, it was very serendipitous,” Dr. Grilli said. “I’m really lucky, actually; it’s hard to imagine another place in the world I’d rather be for an eye repair.”
A damaged “roll of film”
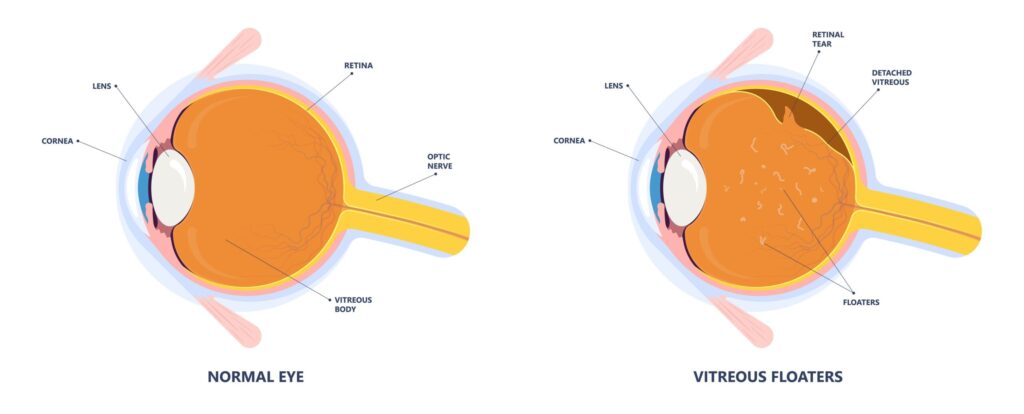
The eye works a lot like a camera. In front of both the camera and eye is the lens, which focuses light to create images on a roll of film and, in the eye’s case, the retina. Using sensory cells on its outer surface, the retina captures light travelling from the front of the eye to its location on the back wall. It then processes the light into signals sent to the brain via the optic nerve.
In the space between the retina and the lens is a gel called the vitreous through which light travels. Over time, the gel degenerates and pulls away from the retina, a process called posterior vitreous detachment. Sometimes, the pull of the gel can tear the retina, which allows fluid to separate the retina from the back wall of the eye.
According to Dr. Kim, retinal tears occur in roughly 10 percent of patients who experience vitreous detachments. However, nearsighted individuals, such as Dr. Grilli, have longer-shaped eyes that can lead to a greater pull on the retina from the gel, making the retina more susceptible to tears. In Dr. Grilli’s case, a tear in the retina, as well as a partial retinal detachment, had occurred. The odd flashes of light he experienced were warning signs from the brain signaling that the retina was under duress.
To fix the retinal detachment, Dr. Kim would need to perform a vitrectomy. The operation requires removing the gel inside the eye, draining the fluid underneath the retina and welding the tear with a laser. A gas bubble is then inserted into the eye where it sits for six-to-eight weeks, serving as a “cast” that holds the retina in place while welding around the tear strengthens.
Addressing two problems at once
Just like any other patient, Dr. Grilli couldn’t help but think of a few worst-case scenarios in the hours leading up to his operation. While good outcomes are expected from the procedure, a patient’s vision is significantly impaired by the gas bubble before it can return to normal. He thought of the future appointments he needed to cancel and the accommodations he would need to make with his family at home. Dr. Grilli also knew his return to the operating room would depend on the success of his surgery and recovery.
“Not only did my vision hinge on the operation’s success, but so did my career,” Dr. Grilli said. “My job is completely hands-on and requires near-perfect vision. Who knew what could happen to my practice if my vision was compromised?”

Complicating matters was Dr. Grilli’s glaucoma. Vitrectomies pose a unique risk for patients with glaucoma, who are unable to adequately drain fluid from the front of their eyes. Steroids prescribed after a vitrectomy can further impede the drainage system, causing pressure in the affected eye to build to levels higher than the elevated pressures people with glaucoma normally experience. If such pressure stays elevated long enough, it can permanently damage the optic nerve.
“I like to think of the optic nerve as the eye’s fiber optic cable to the brain,” said Dr. Solá-Del Valle, who regularly sees Dr. Grilli three-to-four times a year for his glaucoma. “When that cable is irreparably damaged or detached, the brain can no longer receive the strongest, sharpest images possible.”
At Mass Eye and Ear, physicians and surgeons regularly collaborate across a wide array of specialties to produce exceptional results for complicated cases. In Dr. Grilli’s case, Dr. Kim knew she would need to collaborate with Dr. Solá-Del Valle to properly manage any noticeable spikes in pressure and avoid derailing the recovery process.
Collaborating a recovery
After undergoing his procedure in November 2021, Dr. Grilli may have become the first person to ever perform and undergo a surgical procedure at Mass Eye and Ear on the same day. Being a footnote in hospital history did not make his immediate path forward any less daunting, however.
Dr. Grilli needed to spend his first weeks lying face down as much as possible so the gas bubble would stay pressed against his retina. Using a specially designed chair at home, he could only watch television or read out of one eye.

In the meantime, he needed to vigilantly follow the instructions of Drs. Solá-Del Valle and Kim, who had customized a treatment plan that accounted for his glaucoma. Both doctors regularly checked in for any signs of a recurring tear such as flashes or floaters and were always willing to meet with him at a moment’s notice. To prevent any sudden spikes in eye pressure, Dr. Kim would taper Dr. Grilli off his prescribed dosage of steroids as early as possible. Eye drops and medications provided by Dr. Solá-Del Valle would also relieve accumulated pressure as needed.
Slowly but surely, Dr. Grilli regained the quality of life he feared he could have lost. By the time he took his daughter to see the latest Marvel movie in theaters, he was already beginning to schedule appointments in his clinic. Three months after his procedure, he was cleared to perform surgical procedures, but not without a regained perspective of what his own patients might experience on a regular basis.
“I feel like I’ve gained a deeper sense of empathy for my patients,” Dr. Grilli said. “During one of the scariest moments of my life, Drs. Kim and Solá-Del Valle did everything in their power to put my anxieties to rest. That exact approach, I now understand firsthand, is why patients worldwide choose Mass Eye and Ear for their care.”



