Researcher Shizuo Mukai, MD put his eye for design and resourcefulness towards addressing a major need in eye clinics worldwide.
When Mass Eye and Ear ophthalmologist Shizuo Mukai, MD discovered that a patient could not afford an expensive steroid implant, it turned into a creative mission. After doing some research – and digging through the recycling bin – he and his team successfully created a working centrifuge from discarded cardboard that can be used for alternative therapeutic applications.

The device, called the CentREUSE, was developed by a team including Dr. Mukai; Jovany Franco, a Harvard Medical School (HMS) fourth-year student; Tatsuo Nagata, MD, an ophthalmology research fellow from Japan at Mass Eye and Ear and HMS; and Takayuki Okamoto, a Japanese medical student doing an ophthalmology rotation at Mass Eye and Ear and HMS.
Dr. Mukai and Franco described to Focus the need for more accessible medical devices that have historically been too expensive or required specialized materials that are unavailable in underserved areas.
“The CentREUSE can be easily constructed from readily available, discarded materials,” said Dr. Mukai. “This is the first human-powered, portable, ultralow-cost, paper material-based centrifuge to be applied in a therapeutic setting, and we hope this work will inspire others to advance it further to help patients around the world.”
Addressing a need through recycled materials
Patients with eye diseases including diabetic macular edema, age-related macular degeneration or uveitis may benefit from implantable or injectable steroids if their symptoms don’t improve with first-line treatments. The steroid implants are quite expensive and cost between $10,000 and $20,000. In some cases, the injectable steroids that cost about $20 can be processed in a centrifuge, a machine that spins rapidly to enable the injectable steroid to be made into a greater concentration that can approach the effectiveness of the steroid implants. Commercial centrifuges are extremely expensive, and many clinics in the United States and around the world – especially in more resource-poor settings – do not have access to them.
When one his patients could not get insurance approval for an implant, Dr. Mukai brainstormed ways he could centrifuge these steroid suspensions himself. Using a centrifuge from another lab was not an option; often these machines are not clean since they spin urine and blood samples or are used for research purposes, and to inject medication into the eye, the machines have to be clean.
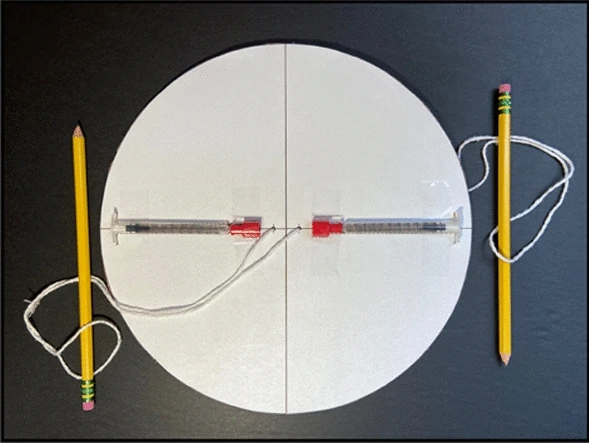
The idea for developing a new, clean, but cost-effective, centrifuge first came from Dr. Nagata, a research fellow working in Dr. Mukai’s lab. After researching similar centrifuges made from non-traditional materials, namely the “paperfuge” developed by Stanford University bioengineers that was inspired by the whirligig toy, the team was confident they too could use recycled materials they had on hand and scale up existing models to a size large enough to accommodate the syringes they needed. They created a model completely out of “trash,” to ensure it could be made anywhere in the world and called it the CentREUSE. They used syringes, a piece of discarded but clean cardboard, string and two pencils that would serve as handles. Lab member Franco then led multiple experiments to determine the efficacy of the centrifuge. Tests revealed that they could achieve the necessary rotational speed and concentrations of steroids needed after spinning by hand that was comparable to what a commercial-grade centrifuge would produce.

“The big selling point of this prototype is that we have a device that permits you to do this directly in a care setting, in a really cost-effective way,” said Franco. “We also wanted to show through our experiments that you’re not sacrificing effectiveness to do it this way.”
Franco was attracted to this project in Dr. Mukai’s lab because it was very different from the conventional research projects most medical students work on, like studying treatment outcomes. His parents are from rural Mexico and he has extended family there, and he said he can envision the CentREUSE benefitting people in communities like the one his family is from.
Dr. Nagata and Okamoto came to Mass Eye and Ear and HMS as part of a longstanding tradition started in the 1960s, where more than 300 research fellows and medical students from Japan have trained. Dr. Mukai, who first participated in this training program starting 33 years ago, said some of these fellows have gone on to become chairmen of ophthalmology departments, and even deans of medical schools after returning to Japan.
“We had a really fantastic team working on this project,” said Dr. Mukai.

The researchers submitted their work to scientific journals, and it was accepted and published in February in Nature Scientific Reports as an open access paper, meaning anyone around the world could access the paper for free. That was important to the team as their hope is that the CentREUSE will be easy to re-create, accessible to all, and inspire others to modify the cardboard centrifuge for other therapeutic and diagnostic applications as well.
“If you can take a $20 bottle of steroids and spin it down and inject it into the eye, versus an implant that can cost 10,000 to 20,000 dollars, that will make a huge difference,” said Dr. Mukai.
An eye for design
While he has not had any formal training in engineering, Dr. Mukai has always had a great interest in design and exposure to instrument development.
“I have a very different background from most ophthalmologists,” said Dr. Mukai “I was an art major in college. I majored in sculpture and photography at Brown University and took design courses at Rhode Island School of Design. One of my colleagues calls me a hippie!”
For many years in high school and college, Dr. Mukai had a summer job working with engineers in the Physics Lab of the Eye Research Institute (now the Schepens Eye Research Institute of Mass Eye and Ear). He worked primarily with Francois Delori, PhD, who invented fundus autofluorescence and is a world expert on light safety of ophthalmological devices. He was also fortunate to be there at the same time as Robert Webb, PhD, who invented the scanning laser ophthalmoscope, Martin Mainster, MD, PhD, a laser expert, and Oleg Pomerantzeff, a bioengineer and physicist who helped legendary ophthalmologist Charles Schepens, MD, design the binocular indirect ophthalmoscope.
“I use the systems and devices they developed every day in my clinical practice,” Dr. Mukai exclaimed.
This experience led him to medical school and a storied career in ophthalmology where he has become a leading expert, including in rare childhood cancers like retinoblastoma. But Dr. Mukai never lost his eye for design. His work also brought him around the world on surgical teaching trips in different continents through Mass Eye and Ear’s Office of Global Surgery. He’d often find many clinics lacked equipment or had broken ones needed for basic procedures and would find himself fixing them. That experience also helped him look towards designing eye care solutions that can be used worldwide.
Thanks to the Mukai Fund, which is a research fund at Mass Eye and Ear supported exclusively through the generosity of donors, he can pursue these projects. Some inventions that have come out of his fund include a smartphone fundus photography system that can examine patient’s eyes without the need to dilate them first and an app that can detect leukocoria, or “white eye” from photos, potentially identifying future cancers.
Dr. Mukai consults on many design projects and enjoys teaching engineering at universities and high schools, in addition to his day-to-day clinical work.
With his inventions, the most important thing to Dr. Mukai is that they are accessible.
“You often hear inventors in our field and others look toward technologies like the 3D printer. Most people don’t have one, I certainly don’t,” said Dr. Mukai. “We aslo hear complaints that many of the papers describing innovative technologies are published in journals that require expensive subscriptions. We want to ensure that our work can be replicated and made very easily, and is open-sourced, where anyone, even high school kids, can find it and improve upon it.”



