Mass Eye and Ear is celebrating its 200th anniversary, and the Focus blog each month will have stories on the hospital’s past, present and future. In March, Focus is spotlighting some of the otolaryngology—head and neck surgery department’s most significant achievements in clinical care, research and education.
Over the past 200 years, the Department of Otolaryngology—Head and Neck Surgery at Mass Eye and Ear has dramatically transformed and developed into the robust department that the world knows today. The hospital has made remarkable strides in patient care, research and education throughout its history. With innovation at its forefront, two centuries of notable growth and success have been achieved.

Clinical and surgical “firsts” through the centuries
In 1892, Frederick L. Jack, MD, at what was then known as the Massachusetts Charitable Eye and Ear Infirmary, became the first doctor in the United States to perform a stapedectomy, an emerging operation that promised to restore hearing in patients with otosclerosis, by removing a small bone called the stapes in the middle ear. Initially, stapedectomies had limited success, but otologists persisted in refining tools and techniques, eventually turning them into an effective surgical treatment. Harold F. Schuknecht, MD, who served as Chief and Chair of Otology and Laryngology at Harvard Medical School and Mass Eye and Ear from 1961 to 1985, played a pivotal role in this progress. In the 1950s, he developed a groundbreaking metal stapes prosthesis measuring just 0.6 millimeters, which revolutionized the field. Dr. Schuknecht quickly gained international recognition as one of the most sought-after stapedectomy surgeons.
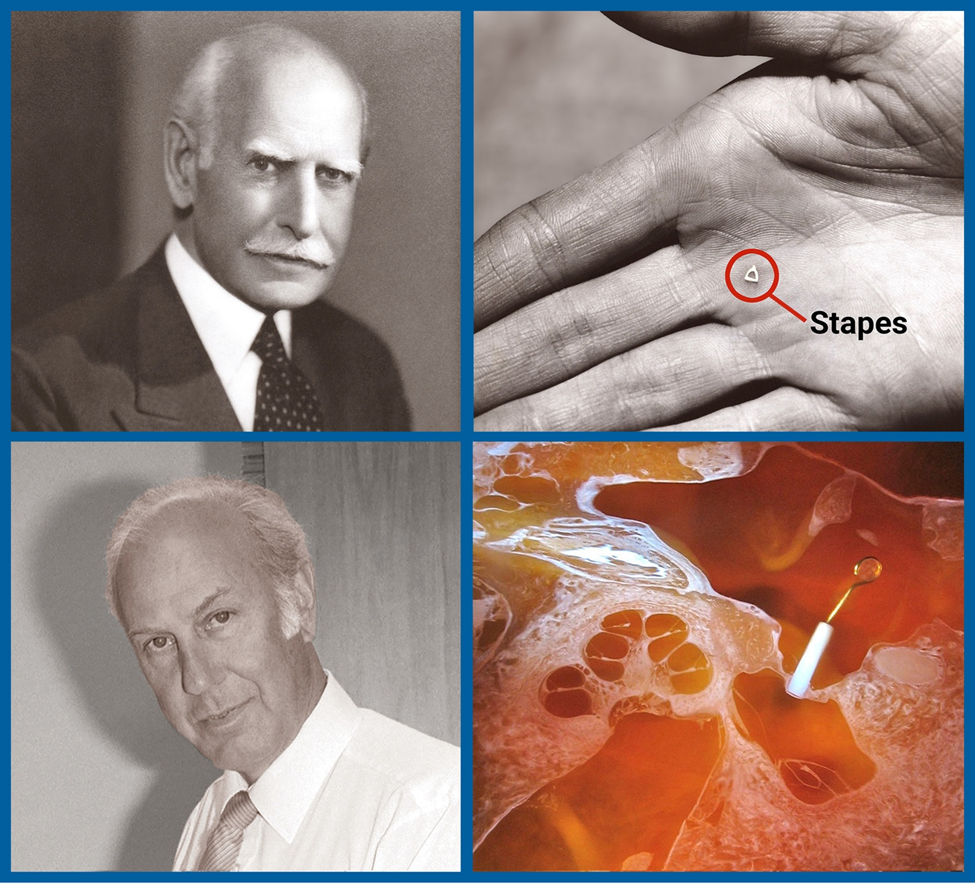
In the 1960s, Philip Meltzer, MD, DMD, who served as Interim Chief of Otology and Laryngology at Mass Eye and Ear, left a notable mark on the refinement of surgical techniques and treatment therapies for otosclerosis-related deafness. He was also well known for developing a technique for the removal of adenoid tissue from the nasopharynx in children, resulting in improved outcomes and reduced complications associated with this procedure.
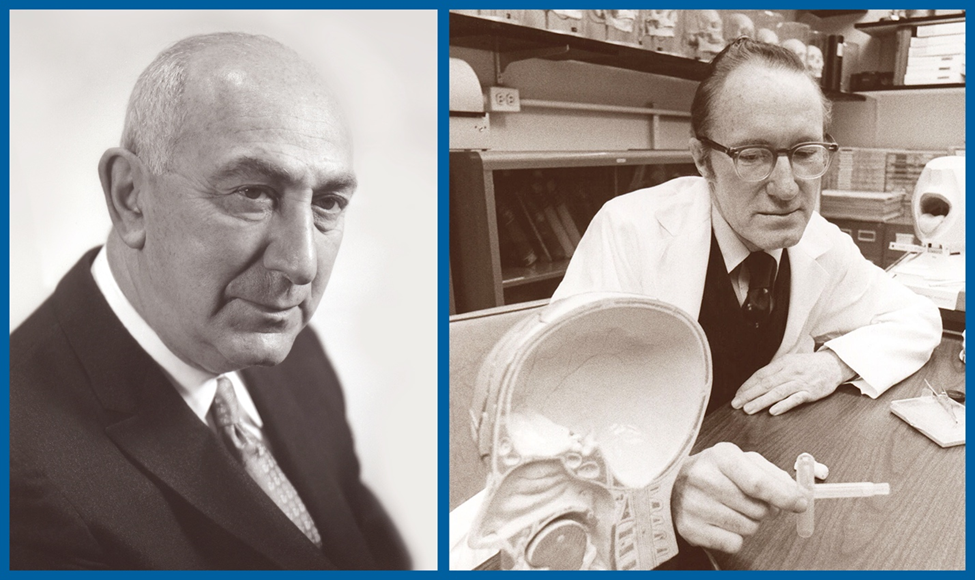
The Montgomery® T-Tube, invented by William Montgomery, MD, former John W. Merriam Professor of Otology and Laryngology at Harvard Medical School, in the early 1970s, stands as one of the most influential innovations in otolaryngology. Dr. Montgomery was initially motivated to create a solution to tracheal collapse after treating a patient at Mass Eye and Ear who had suffered a crushed trachea from a car crash. The conventional approach to this injury was to perform a tracheotomy or opening a hole in the trachea for the patient to breathe. Unfortunately, that procedure for this level of injury did not provide relief and often left patients without a voice and or ability to breathe through the mouth.
With this in mind, Dr. Montgomery developed a new approach. Using two pieces of porcelain, he began by building a T-Tube prototype. He then developed a procedure that reconstructed the trachea with local soft tissue and used the T-Tube to keep the airway stable, allowing the patient to breathe and speak while healing from the tracheal reconstruction. Today, the updated version of the T-Tube is the most commercialized item in the history of Boston Medical Products.
Around 10 years later in 1984, Joseph Nadol, Jr., MD, a trailblazer in the surgery and pathology of the ear and temporal bone, performed the first cochlear implant surgery in New England. Dr. Nadol, Walter Augustus Lecompte Professor and Chair of Otology and Laryngology at Harvard Medical School and Chief of Otology and Laryngology at Mass Eye and Ear and Mass General Hospital from 1985-2013, successfully implanted the device into the ear of patient John F. Anderson, Jr., restoring his hearing.

In 1993, Dr. Montgomery collaborated with Mark A. Varvares, MD, FACS, current Chief of Otolaryngology–Head and Neck Surgery at Mass Eye and Ear and Massachusetts General Hospital and John W. Merriam/William W. Montgomery Professor and Chair of Otolaryngology–Head and Neck Surgery at Harvard Medical School, on a novel thyroplasty implant designed to be utilized as part of a surgical operation that achieves medial displacement of a paralyzed vocal cord. After a decade of research and successful clinical experience, the Montgomery® Thyroplasty Implant System was patented as a safe and effective device used for treating unilateral vocal cord paralysis. This revolutionary system eliminated the time-consuming process of customizing implants during surgery.
Thirty-six years after the inaugural cochlear implant procedure in New England, Daniel Lee, MD, FACS, Director of the Pediatric Otology and Neurotology Division, successfully performed surgery on Luna, the youngest child – six months old — to undergo bilateral cochlear implants at Mass Eye and Ear after being born with profound deafness [watch Luna’s story].

In 2022, Christopher Hartnick, MD, MS, Director of the Division of Pediatric Otolaryngology at Mass Eye and Ear, released the results of a clinical trial in adolescents with Down syndrome testing a hypoglossal nerve stimulator. After showing dramatic reductions in sleep apnea, the device received FDA approval for this age group in this underserved population.

Research “firsts” through the centuries
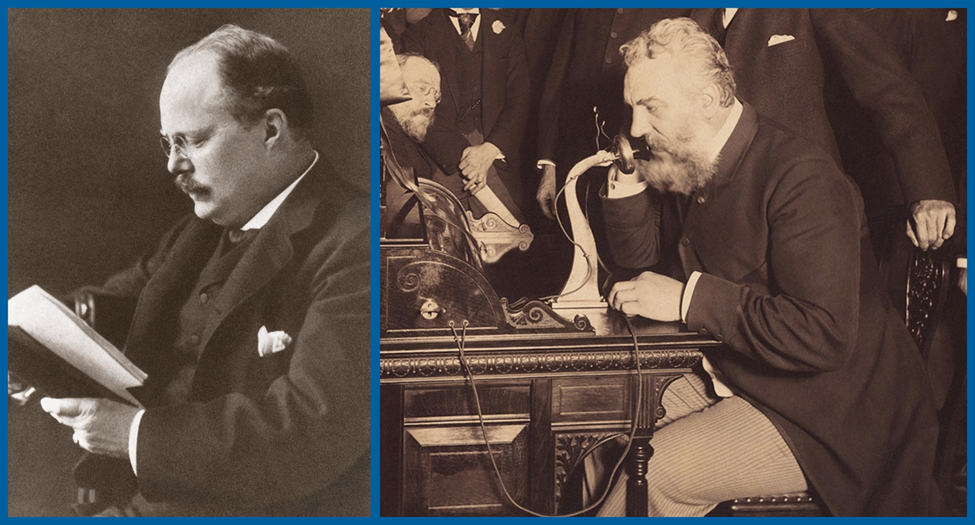
In 1871, Alexander Graham Bell was seeking to understand if vibrations in the air produce sounds heard by the human ear, with a hope to perfect a device used to record sound. He collaborated with Harvard Medical School’s inaugural Professor of Otology and the Massachusetts Charitable Eye and Ear Infirmary’s Chief of Aural Service, Clarence Blake, MD, to further investigate this question. Meeting in Boston, Dr. Blake provided a dissected human temporal bone for Bell to observe the anatomy of the middle ear which helped give Bell the idea of a membrane speaking telephone.
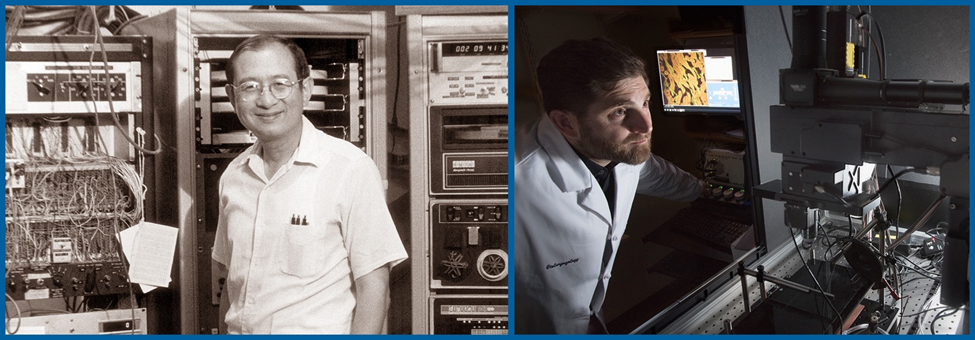
In 1958, Nelson Yuan-sheng Kiang, MD, PhD founded the Eaton-Peabody Laboratory of Auditory Physiology, which originally was established as a multidisciplinary laboratory. Now known as the Eaton-Peabody Laboratories (EPL), it is located within Mass Eye and Ear and stands as one of the largest and most established auditory research centers globally. Housing 16 independent federally funded laboratories, EPL works on a full spectrum of hearing research questions. Research is organized into five related categories: inner ear biology, acoustics and biomechanics, central auditory processing, tinnitus and audiology research. In 2022, Daniel Polley, PhD, was named Director of the EPL.
In the 1960’s, Dr. Kiang was credited as the first to demonstrate the auditory brainstem response, and to propose using such electrical signals from the brain to diagnose hearing disorders. He was also a pioneer researcher on sound coding in the auditory nerve. This work earned him international recognition and was critical for understanding and developing treatments for hearing-related conditions.
In the 1970’s, Drs. Nadol and Kiang recruited Aaron Thornton, PhD, CCC-SLP/A to Mass Eye and Ear to establish the Auditory Evoked Response Laboratory. Soon after, Barbara Herrmann, PhD, joined the lab, and she and Dr. Thornton, both audiologists and clinician-scientists, worked together to develop a novel device capable of detecting auditory brainstem responses in infants. At the time, the average age of identifying pediatric hearing loss was two-to-three years, and few otolaryngologists knew how a delayed hearing diagnosis could affect a child’s ability to speak and understand language. With the encouragement of Dr. Nadol, the duo partnered with Ronald Eavey, MD, former Chief of Pediatric Otolaryngology at Mass Eye and Ear and opened their research lab to pediatric patients in the Neonatal Intensive Care Unit at Massachusetts General Hospital (MGH). They were able to screen several infant patients, which gave them enough data to confirm that their technique could accurately detect hearing loss in children less than six months of age. By 1985, Drs. Thornton and Herrmann had worked with a startup company to develop their hearing screener into a commercialized product, which is sold worldwide to this day.

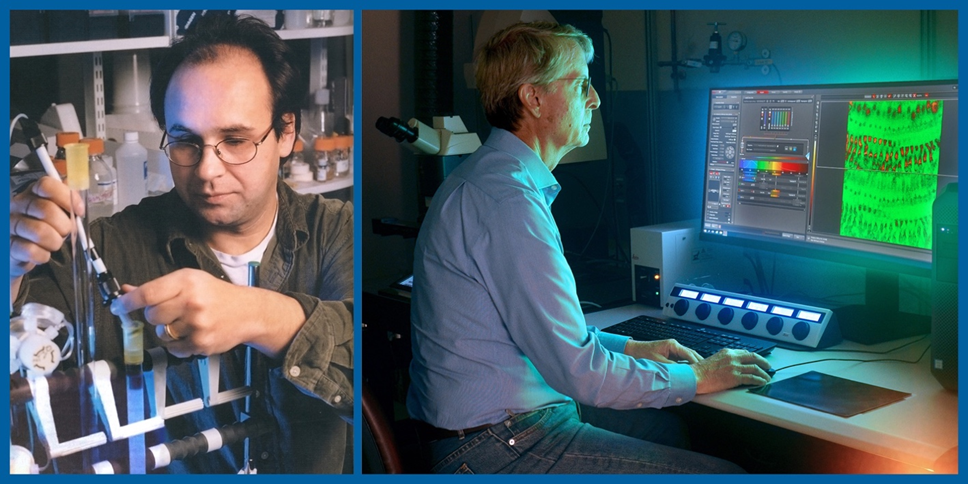
In 2003, a research team led by Stefan Hellar, PhD, previous principal investigator at the EPL and assistant professor at the Department of Otology and Laryngology at Harvard Medical School, had discovered a new population of stem cells in the inner ear, that can be converted to hair cells, in adult mice. This finding unlocked new potential treatments for hearing loss for decades to come.
In 2009, M. Charles Liberman, PhD, co-discovered a phenomenon called cochlear synaptopathy, also referred to as “hidden hearing loss,” a pivotal discovery that has since informed the global understanding of the causes of hearing loss. Thirteen years later, Dr. Liberman was awarded the 2022 Scientific Grand Prize from the France-based La Fondation Pour l’Audition. The award is one of the highest honors given in hearing science. Dr. Liberman is the Harold F. Schuknecht Professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School, and previously served as the Director of the EPL for more than 25 years, where today he remains an investigator.
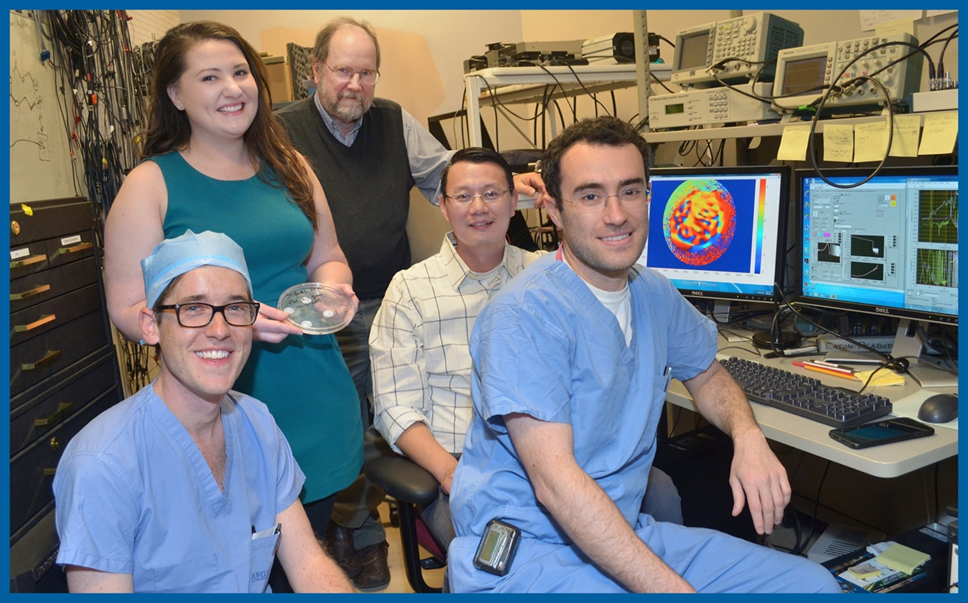
After the 2013 Boston Marathon bombing, Mass Eye and Ear Emergency Department clinicians (both ophthalmology and otolaryngology–head and neck surgery) responded to dozens of patients. This experience inspired future research efforts including developing an experimental method to repair ruptured eardrums with 3D printing, called the PhonoGraft, co-spearheaded by Aaron Remenschneider, MD, MPH, and identifying a promising biomarker for tinnitus, led by Daniel Polley, PhD.
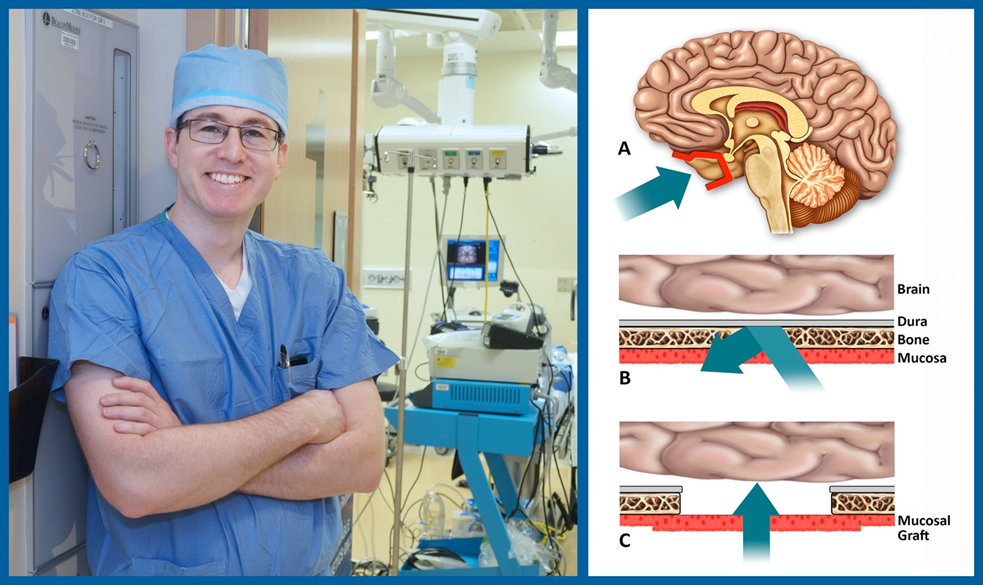
In 2015, a research team led by Benjamin Bleier, MD, Director of Otolaryngology Translational Research at Mass Eye and Ear, successfully discovered new techniques to deliver drugs across the naturally impenetrable blood-brain barrier in a Parkinson’s mouse model. These significant findings were a major step towards the treatment of Parkinson’s disease, which would bring hope to patients around the world who struggle with this condition.
Kristina Simonyan, MD, PhD, DrMed, Vice Chair of Clinical Research, led a trial in 2020 using artificial intelligence (AI) to diagnose dystonia, a first-of-its-kind technology to enable fast and accurate diagnosis for this debilitating disease. This work led to a later research project in 2022 that used AI to determine which dystonia patients could most benefit from Botox injections, a treatment that is not effective in every patient.
In January of Mass Eye and Ear’s bicentennial year, 2024, Zheng-Yi Chen, DPhil, an Associate Scientist in the EPL, published results from a clinical trial with the Eye & ENT Hospital of Fudan University in Shanghai, China, in which five of six children who were born with an inherited form of deafness caused by mutations of the OTOF (otoferlin) gene, called DFNB9, and were treated with an experimental gene therapy, had recoveries in their hearing, and dramatic improvements in speech perception and conversational abilities. This research represents the first human clinical trial to administer gene therapy for treating this condition, with the most patients treated and longest follow-up conducted to date.
Educational “firsts” through the centuries
In 1879, the Board of Managers opened a clinic for teaching otology to Harvard Medical School students in a converted patient waiting room, and shortly after Dr. Blake was appointed as the first professor and chairman of the Harvard Medical School Department of Otology and John Orne Green, MD, was named professor of clinical otology. In 1900, Harvard Medical School otolaryngologic instruction found a home at Mass Eye and Ear, where it remains today.
Soon after, The Mosher Course, a famed postgraduate program in head and neck anatomy at Harvard Medical School (commonly known as the “Friday Night Course”), was established by Harris Peyton Mosher, MD, who served as its instructor from 1903 to 1939. Dr. Mosher was named Chief of Laryngology in 1920 and from 1932-1939 he became the sole Chief of both Otology and Laryngology. Additionally, he played a pivotal role in the establishment of the American Board of Otolaryngology and served as its President for 22 years.
Varaztad Kazanjian, MD, DMD, joined Massachusetts Eye and Ear Infirmary (MEEI) in 1923 and played a critical role in founding the subspeciality of facial plastic and reconstructive surgery and led the combined MEEI/MGH Plastic Surgery Clinic. In 1941, he became the first professor of Plastic Surgery at Harvard Medical School. Originally trained as a dentist, he expanded his practice dealing with facial injuries in a field hospital during World War I, as a member of the first Harvard Unit of the British Medical Corps, which was part of the British Expeditionary Forces in France, where he helped develop the practice of intermaxillary fixation. He treated more than 3,000 cases of gunshot, shrapnel and other severe wounds of the face and jaws and became known as “The Miracle Man of the Western Front.”
Since the 1960s, Dr. Schuknecht mandated research participation for all residents. He conducted otopathology teaching sessions on Sunday mornings, guiding trainees through microscopic anatomy training until they could visualize the presumed structural changes in the inner ear underlying clinical signs and symptoms. Many future distinguished otology leaders were first introduced to these concepts in the renowned “Sunday School.” Around this time, Dr. Schuknecht also established the Otopathology Laboratory at Mass Eye and Ear. Since its inception, the Otopathology Laboratory has been a basic and translational human temporal bone pathology laboratory with a mission to improve the diagnosis and treatment of disorders causing hearing loss, balance dysfunction and facial paralysis. In 2021, Alicia Quesnel, MD, was named the first female director of the Otopathology Laboratory.
Dr. Kiang was a mentor to dozens of students and young investigators as a Professor of Physiology at Harvard Medical School. His passion for education was further realized in 1992, when he spearheaded the creation of a PhD program in Speech and Hearing Biosciences and Technology (SHBT), which is now a part of the Division of Medical Sciences at Harvard Medical School. Several of the Harvard Department of Otolaryngology—Head and Neck Surgery’s faculty teach these courses to this day, and many of the post-doctoral students work in the department’s labs.
In the last few decades, the Harvard department has implemented several Continuing Medical Education (CME) courses that are conducted on an annual or biennial basis. In support of improving patient care, Harvard Medical School is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), to provide continuing education for the healthcare team.

The courses taught from 1996 onwards include:
- Surgery of the Thyroid and Parathyroid Glands
(Director: Gregory Randolph, MD, FACS, FACE) - Update in Head and Neck Cancer
(Co-Directors: Jeremy Richmon, MD and Daniel Deschler, MD, FACS) - Endoscopic Surgery of the Sinuses, Eustachian Tube, and Ear
(Director: Ralph Metson, MD) - Comprehensive Otolaryngology Update
(Director: Nicolas BuSaba, MD, FACS) - Snoring and Sleep Disordered Breathing – Evaluation and Management
(Director: John Dobrowski, MD, FACS) - Sialendoscopy Symposium
(Director: Wais Rahmati, MD, MPH, FACS) - Technology and Innovation in Endocrine Head and Neck Surgery
(Director: Gregory Randolph, MD, FACS, FACE)
In 2019, the department changed its name to Harvard Medical School Department of Otolaryngology–Head and Neck Surgery to be consistent with how the specialty is known nationally. Over the past several decades, the department has been a collaborative effort between five clinical venues: Mass Eye and Ear, Massachusetts General Hospital, Beth Israel Deaconess Medical Center, Brigham and Women’s Hospital and Boston Children’s Hospital. These institutions provide comprehensive subspecialty training in otolaryngology, including exposure to head and neck oncology; facial plastic and reconstructive surgery; thyroid and parathyroid surgery; rhinology; laryngology; otology and neurotology; and pediatric otolaryngology.

Celebrating the past; simultaneously looking ahead
Over the past two centuries, the Department of Otolaryngology—Head and Neck Surgery has had many “firsts,” and Mark A Varvares, MD, FACS, Chief of Otolaryngology–Head and Neck Surgery at Mass Eye and Ear and Massachusetts General Hospital and John W. Merriam/William W. Montgomery Professor and Chair of Otolaryngology–Head and Neck Surgery at Harvard Medical School, is confident there are many more to come. The department continues to evolve and expand, with faculty and staff dedicated to its four core pillars: delivering compassionate care, pioneering research, training tomorrow’s medical leaders, and engaging in community service.
“Our bicentennial year is an opportunity to reflect and commemorate 200 years of groundbreaking innovation, while simultaneously looking ahead to a brighter future for patients with diseases of the ear, nose, throat, head and neck,” said Dr. Varvares. “As we celebrate our history and recall its remarkable evolution, our unwavering commitment to our mission remains paramount.”