In April 2020, the Greater Boston region was experiencing the peak of a COVID-19 outbreak. Mass Eye and Ear transformed the 10th floor inpatient unit into an acute medical unit to care for patients who were recovering from COVID-19 after being released from the Intensive Care Unit at neighboring Massachusetts General Hospital (MGH).
Dr. Michael Wu, a second-year Otolaryngology–Head and Neck Surgery (OHNS) resident, was one of several Mass Eye and Ear clinical trainees who volunteered to staff the COVID-19 recovery floor at the height of the pandemic. He shared his experience with Focus.
Where were you working when the pandemic began?
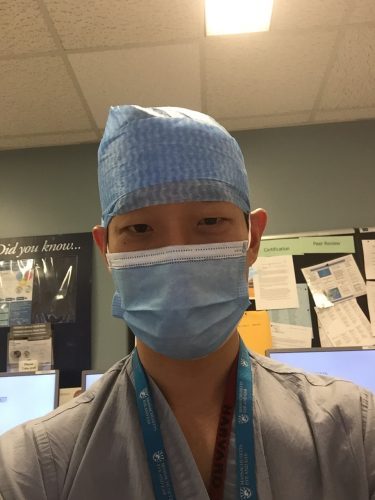
When COVID started really hitting the U.S., I was a first-year resident. First-year interns are usually assigned or “on loan” to other services – to general surgery, neurosurgery, plastic surgery, you name it. At the time, I was in the general surgery service at Mass General Hospital (MGH). The general surgery department made the decision to re-deploy many of its residents to assist in the COVID-19 response. After starting in surgery, I ended up working the internal medicine overnight shift on the general inpatient floor for COVID patients. I was able to work alongside all sorts of interesting people who I normally would not be working with as an OHNS resident. I worked on the MGH COVID floor for a few weeks, and then on and off in the COVID unit at Mass Eye and Ear for about a month.
How would you describe your experience in the COVID units at Mass Eye and Ear and MGH?
Hospitals were quickly filling up at the height of the pandemic, and there became a need for a rehabilitation facility for COVID patients to go to recover. Luckily, Mass Eye and Ear provided an easy “in-between” destination for recovering patients from MGH. I was on the COVID unit at Mass Eye and Ear for about one month, and we had one OHNS and one Ophthalmology resident on at one time. We don’t often get to see the other Ophthalmology residents, so it was nice to be able to make some new connections within our hospital and work together to take care of patients. It was a slower pace than the previous floor I was on at MGH during the surge, but it was very rewarding to see patients improve and be able to go home. In addition to meeting Ophthalmology interns, it was great being able to work alongside the physical and occupational therapists who were deployed to Mass Eye and Ear from MGH, and were instrumental in patients’ recoveries.
What were your key takeaways from your time in the COVID units?
The acuity of the surge was a very interesting experience. Early on, we were very aware of how quickly the patients’ conditions could worsen. There was a very low threshold for intubating patients. It was very dramatic and stressful at times. I would be on the phone in full PPE, often using a translator, making calls in the middle of the night to tell family members that a patient needed to be intubated.
This pandemic definitely puts things into perspective. During residency, you can become jaded or lose sight of why you decided to go into this field in the first place. It was also humbling as someone in the medical field; sometimes we have that invincible mentality, but we were seeing first-hand that this virus does not discriminate – you could be old, young, with preexisting conditions or perfectly healthy. I was also struck by the burden of COVID-19 on our local Hispanic community, which has since been well-documented.
It was incredible to not only see the entire medical community come together, but our neighborhood community as well. I can’t tell you the amount of food donations we received at the hospital, frequently from establishments that were struggling themselves during the pandemic. Those meals were so appreciated. We’re not out of the woods yet, but I hope everyone continues to see that kind of positivity.
Read more for the experience of one of our Ophthalmology residents, Dr. Karen Wai.



